Is What’s Good for “Everybody” Always Good for Us?
Opinion Editorial by Phill Wilson
In order for the Black community to end the AIDS epidemic, we must all assume individual responsibility for taking care of our health. Sometimes this means going to the doctor for an annual checkup. Sometimes it means getting an HIV test. But you can't take care of yourself if you don't know what steps to take. Many of us need to know more.
This week we ask questions about a very important self-care step that women can take to prevent sexually transmitted diseases (STDs) and cervical cancer.
In "The New Pap Smear Guidelines: Are They Right for Black Women and Girls?" we ask Elizabeth Bradley, M.D., vice chair of ob-gyn at the Cleveland Clinic, whether the dramatic changes in Pap smear guidelines issued by the American College of Obstetricians and Gynecologists (ACOG) are good for Black women and girls. While we understand why the changes could be positive overall, we have good reason to be concerned. One reason: ACOG's recommendations include one that would raise the age at which a young woman obtains her first Pap test to 21--no matter how old she was the first time she had sex. A Pap smear helps doctors test for human papillomavirus (HPV), the STD that can cause genital warts, cervical cancer and other sexual-health problems.
With an STD epidemic raging among Black folks--for example, research shows that 50 percent of Black teenage girls have an STD, by far the highest rate of any race--might such a delay unintentionally negatively affect our community, perhaps contributing to the further spread of STDs? Or are the benefits of waiting until 21 that ACOG describes (for example, fewer invasive medical procedures performed on our teens) worth the risk? If ACOG is right, are there alternative ways for sexually active teens and young women to protect themselves until they turn 21? And if you already have HIV, do other changes in the guidelines apply to you?
These questions are critically important in the fight against AIDS, since people who have one STD not only are more likely to become infected with HIV if they’re exposed to it--STDs weaken the immune system--but are also more infectious to others if they already have the HIV.
As you'll learn, determining how these questions apply to your individual situation isn’t always straightforward or easy. But by becoming informed, each woman can take the appropriate steps to protect her health and, by extension, that of our community. When we know better, we do better.

The New Pap Smear Guidelines: Are They Right for Black Women and Girls?
The American College of Obstetricians and Gynecologists (ACOG) recently released a revised set of recommendations about Pap smears, which screen for cervical cancer. Doctors now suggest that women get their first screening when they turn 21 instead of within three years of becoming sexually active. They also recommend that the tests be done less frequently--every two years instead of every year.
While most health experts have signed off on the plan, others question whether it's the best idea for Black girls and women, since there is an STD epidemic in the Black community and recent research shows that about 50 percent of Black teenage girls have an active STD. We asked Linda Bradley, M.D., vice chair of ob-gyn at the Cleveland Clinic, the reasons behind the changes and whether there are exceptions that we need to be aware of.
"This is about new scientific information being available," says Dr. Bradley. "Physicians now have more information to guide them in making recommendations about the frequency of a Pap smear--information about the natural history of cervical cancer and [its relationship] to the human papillomavirus (HPV). We're learning, for instance, that some women have a 'double-negative Pap smear,' which means you are so unlikely to develop precancer that doctors can defer tests unless you have been previously diagnosed with HPV."
This is key, Dr. Bradley says, because overtesting could lead to unnecessary procedures that may put a woman's health at risk. "In the past when we've seen patients with HPV, [sometimes] we took out their cervixes. That type of unnecessary treatment of adolescents, for instance, can lead to infertility later--the female may not be able to conceive or could have a premature birth."
Still, Dr. Bradley warns, Pap smear testing every two years beginning at 21 is absolutely crucial--not just to evaluate the health of the cervix but to allow a doctor the opportunity to check for any other possible health issues as well. ACOG states that women and girls who have been vaccinated against HPV follow the same guidelines as those who have not.
"See your health care provider on an annual basis," she continues. This advice also applies to teens and adolescents. "There are other things that doctors do--they check your blood pressure, ask about STDs, [may] test for HIV, give pelvic exams and look for fibroids, test your cholesterol, give nutrition recommendations....African American women are disproportionately at risk for a number of these health issues."
Women 30 years old and up, she adds, need a Pap smear only once every three years if they've had three consecutive normal, negative Pap smears in a row.
Yet the new recommendations don't apply to everyone. "What we're operating with here are just guidelines," she says.
One exception? Young women and girls who begin having sex in their teen or preteen years need to be checked for cervical cancer long before they turn 21. (Your daughter's health provider should recommend when.) "You won't know whether or not you have HPV until you get tested for STDs," says Dr. Bradley. "In order for us to properly assess risk, patients must be honest with their doctors about their sexual histories."
Also, women at higher risk for cervical cancer should get a Pap test every year. This group includes those who are HIV-positive, have had cervical cancer or have been exposed to diethylstilbestrol (DES), a drug once used to suppress lactation as well as to treat advanced breast cancer in postmenopausal women.
In the end, Dr. Bradley says, knowledge is power. Women must familiarize themselves with the new Pap smear guidelines, and if they fall into any of the categories of exceptions described, they should be tested at a younger age or more frequently than once every two years. Women who are not certain that their sexual partners are STD-free (including HIV-negative) or do not use condoms consistently should talk to their doctor about how often they need to be seen—and women who experience symptoms such as bleeding after intercourse, spotting between periods or pelvic pain should call their health care provider immediately.
"And if an older patient comes in with postmenopausal bleeding, you better believe we're going to do a Pap smear on her," she says.
But ultimately, the onus is on the patient to protect herself from STDs and keep up with her own examinations and test results, says Dr. Bradley. "Keep a journal," she says. "Months and years can slip by. Put those dates down in your calendar now so you don't forget."
So while many Black women can follow ACOG's general recommendations, it's probably safest to talk to your doctor about how often you should be tested. And always--always!--use condoms.
Tomika Anderson is a freelance writer whose work has appeared in POZ, Real Health, Uptown and Essence magazines, among others.
AIDS Campaign Targets Neglected Segment of Black America
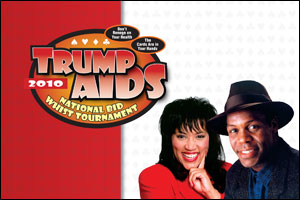
More than a third of new HIV infections in the U.S. occur in people over 40 years old. Yet there have been very few campaigns targeting this population. The Black AIDS Institute, the nation’s only think tank devoted exclusively to combating AIDS among African Americans, is about to change that.
The Institute has found an innovative way to help Black people ages 40 and up become more aware of the HIV/AIDS risk among people their age, while simultaneously raising money to fight the disease in Black communities. The campaign, supported by local organizations, is called Trump AIDS. It leverages the traditional Black pastime of bid whist, a popular card game among Black Americans aged, as a unique way to convene and educate this often overlooked HIV/AIDS demographic.
Trump AIDS will launch in Atlanta, Georgia, on Martin Luther King Jr. weekend, January 15 – 17, 2010 at the Clarion Hotel. The Atlanta event is the first of 30 tournaments and health fairs being held across the nation between January and October, and will culminate with a national bid whist tournament and health fair in Las Vegas, Nevada. For a complete list of cities hosting events and to register, please visit www.TrumpAIDS.org.
“AIDS does not only affect a select demographic such as youth, women or gay men,” says Actor and AIDS Activist Danny Glover, who is a celebrity co-chair of Trump AIDS. “It affects all groups of people. That is why Trump AIDS is such an important campaign for Black people to support and participate in.” Jackée Harry, the other celebrity co-chair, adds, “We must unite as a community—for the sake of our community. To do nothing is to be part of the problem.”
The Atlanta kick-off event will include a Bid Whist Qualifying Tournament and Health Fair in partnership with local Atlanta organizations The 7No! Players, Sister Love and AID Atlanta.
“The 7NO! Players are excited to host the kick-off event in Atlanta,” says Montez Collins, President, 7NO! Players.
“We look forward to welcoming all of our regular bid whist players and any new comers who are interested in learning more about the game.”
“We are proud to partner with the Black AIDS Institutive on this new and innovative awareness campaign to reach Black Americans,” says Sister Love Founder and President Dazon Dixon-Diallo. “When two-thirds of the new HIV/AIDS cases among women in the US are Black, now more than ever it’s important to educate and reach every demographic of the Black community.”
The Health Fair features free onsite HIV testing for all Tournament attendees, players and guests. All are welcome to attend.
The winner of the Atlanta tournament automatically qualifies for a national tournament to be held in Las Vegas in November and a chance to win $45,000.00 in prizes. Other participants can qualify for the national tournament and have their travel expenses to Las Vegas paid by raising $3,000. The participants who raise the most money also get to play in a celebrity tournament.
“Rates of HIV in persons over 50 years of age are 12 times higher among African Americans than among whites,” according to Timothy G. Heckman, Ph.D. “Older people do not consider themselves at risk. Physicians rarely talk to older patients about sex or other risk behaviors.”
“Trump AIDS is an unprecedented event that will provide Black people who are not actively engaged in the HIV battle with access to important health information,” says Black AIDS Institute COO Aron Myers. “This is a tremendous opportunity for the Atlanta community and good citizenship for all.”
“There’s no way to end the AIDS epidemic in Black communities without targeting this population,” adds Black AIDS Institute founder and CEO Phill Wilson. “The Black AIDS Institute has spent the last decade meeting Black folks where they are. Trump AIDS is a perfect example of identifying an indigenous pastime in our community and using it to deliver culturally effective messaging. Everything about this effort, from the date and city where we launch the campaign to celebrity co-chairs—Danny Glover and Jackée Harry—celebrate the Black experience.”
Participants will be encouraged to become involved in the fight to end the AIDS epidemic in the Black community while having fun and potentially winning prizes.
Trump AIDS is a service mark of the Black AIDS Institute.
Rumor Control: Can Men Get HIV From Women?
Absolutely, says Adaora Adimora, M.D., professor of medicine at the University of North Carolina at Chapel Hill School of Medicine and professor of epidemiology at the Gillings School of Global Public Health. "Although it's easier for men to give HIV to women," she says, "HIV transmission from women to men is common."
Roughly a quarter of HIV infections among Black men result from having sex with HIV-positive women, according to the Kaiser Family Foundation. In fact, after sex with other men and IV-drug use, heterosexual sex is the third-most-common method of HIV transmission among Black men, the Centers for Disease Control and Prevention reports.
But men can protect themselves from getting HIV from women. It just requires a little more thoughtfulness and a little less spontaneity. Here are the best strategies:
- Wear condoms consistently (with every single sexual act) and correctly (put one on before your penis touches your partner's skin--yes, including her mouth). Some STDs, all of which facilitate HIV transmission, can spread through any skin-to-skin contact with the infected area.
- Have unprotected sex only with women whom you are certain are STD-negative (including HIV), and only after you've agreed that you will be sexually monogamous--that neither of you will have additional sexual partners while you're having sex with each other.
- Get tested regularly and treated promptly for any STDs. If you're in a monogamous relationship, time your checkup to coincide with your lady's.
Also keep in mind the following:
Even with condoms properly strapped and snapped, certain types of sex are less risky than others. From the riskiest to least risky: anal, vaginal and then oral sex.
Male circumcision has also been shown in African trials to reduce the risk of HIV transmission from women to men. However, that may not be as much of a factor in the United States, where circumcision is already the norm: More than 70 percent of Black men in the United States are circumcised (compared with nearly 90 percent of White men). Still, Black men and women account for more than half of all new HIV infections. While it's a good idea for parents to circumcise their boys, Dr. Adimora cautions against getting "the impression that circumcision will make them bulletproof."
And just how did the urban legend that men can't get HIV from women begin? Dr. Adimora hasn't a clue. But no matter its origin, she says, "It is clearly incorrect."
Carla Murphy, a freelance journalist based in New York City, is a 2009 IPPY Award winner.

FDA Approves HPV Vaccine for Boys and Young Men
About two years ago, Nashville physician Valerie Montgomery-Rice, M.D., decided that her daughter, then 14, would be vaccinated against the human papillomavirus (HPV), one of the most common sexually transmitted infections. (Most people living with HPV don't even know they have it.) The STD--which has more than 100 strains that can infect the genitals, mouth and throat--is especially dangerous for women because some strains are linked to cervical cancer.
The Food and Drug Administration had approved Gardasil a few years ago to prevent cervical, vulvar and vaginal cancer caused by HPV strains 16 and 18; it also prevents genital warts, typically caused by strains 6 and 11. Dr. Montgomery-Rice, a Meharry Medical School ob-gyn, also encouraged her nieces and female patients to get the inoculation, which experts recommend for females ages 9 through 26.
But in October, the government also approved Gardasil to prevent genital warts in males ages 9 through 26, and included it for boys in the federal Vaccines for Children Program.
Now Dr. Montgomery-Rice is having discussions with her son, 14, to get him treated this summer.
The Need to Protect Our Sons In speaking with her son, the doctor is joining a growing chorus of physicians, community-health advocates and others who believe that boys--and young men--should also receive HPV vaccinations.
Research shows that among men who are not already infected by HPV strains 6 and 11, Gardasil is nearly 90 percent effective in preventing genital warts. About 6 percent of all U.S. adults are infected with genital warts.
The drug, which doesn't treat or cure HPV if you already have it, is administered in three injections over a six-month period. Headache, fever and pain at the injection site, along with itching, redness, swelling and bruising, are the most common adverse effects.
Some girls have passed out after receiving the shot. And a small number of severe negative reactions have been reported, including blood clots; however, researchers have been unable to link them directly to the vaccine. Generally the HPV vaccine has been hailed as wonderful.
What's Good for the Goose… Treating men is very important because protecting women is only half the job, says Jean Bonhomme, M.D., a physician with the National Black Men's Health Network, based in Atlanta. Dr. Bonhomme argues that men's health also affects women, so health providers must "address the presence of the virus in both genders," he says. "If the vaccine keeps men safe, then it keeps women safe too."
Even if all infected girls get vaccinated, they can be reinfected from unvaccinated males. Since men don't have a cervix, there is no Pap smear for men. Unless they have symptoms--and they frequently don't--many males might never know they carry HPV and could risk passing it along to their female sex partners. This is particularly problematic because for years, researchers have reported that individuals infected with STDs, including HPV, are at greater risk of both acquiring and transmitting HIV, another STD.
That's why Bill Robinson, a health educator with the Black Men's Health Initiative, makes the recommendation, "Give the vaccine to men." Robinson's North Carolina-based nonprofit brings health messages, including HPV information, to barbershops, churches, free clinics and other grassroots groups.
"When something is good for women, men should not be left out of the equation. With gender, we tend to help one at the expense of the other. If Gardasil is proven effective and prevents a comparable illness in men, we need to consider its use," says Robinson.
Cecily Jones, M.D., an ob-gyn at Dallas's Trinity Women's Center, agrees that the conversation about the vaccine should broaden. "Word needs to get out that a vaccine is out there. Once you're exposed to these strains of HPV, the vaccine's not helpful anymore."
Ervin Dyer is a writer who covers the African-disapora.