When You Know Better, You Do Better
For the last three years or more, I have been saying, "We have the tools to end the AIDS epidemic in America". Now I'm not so sure.
Tonight at midnight The Black AIDS Institute will release a new report, "When We Know Better, We Do Better: The State of HIV/AIDS Science and Treatment Literacy in the HIV/AIDS Workforce," containing the results from the U.S. HIV Workforce Knowledge, Attitudes, and Beliefs (KAB) study, the largest study ever conducted of non-medical personnel working in HIV/AIDS in the United States.
The results of the report are shocking. The more than 3600 respondents from 48 states, D.C., and U.S. territories who participated in the study answered only 63 percent of questions correctly. If this were an academic exam, they would have earned a "D". Said another way, our nation's case managers, social workers, prevention educators, testers and counselors, public health workers and advocates, policy makers, contractors, volunteers and others working in HIV/AIDS are woefully unprepared to help us end our nation's HIV/AIDS epidemic.
For more details read our feature story describing the survey results, as well as our pieces on why science literacy matters and why the HIV workforce is vital to helping us reach an AIDS-free generation. (Click here after midnight tonight to download the report itself.) Beginning Friday the Black AIDS Institute will launch the #KnowBetterDoBetter tour to share the survey data for 10 different cities with the public and the media.
Indeed, all the bio-medical and scientific breakthroughs in the world aren't worth anything, if people working in the HIV field don't understand them, believe in them and know how to use them. This study shows that we are leaving our most valuable resource behind. We have a large infrastructure of passionate, committed and capable people working in AIDS service organizations, community based organizations, clinical settings and health departments ready to get the job done. But they can't do it unless they have the familiarity, knowledge and skills needed to use these new tools.
I have been living with HIV for over 35 years. Every night I take the ARVs that keep me healthy and keep me alive. My regimen is three pills once a day. And you know what? I look at those pills every day and there's one thing that I notice: Not one of them has a way to get into my body without my assistance. What the pills do is biomedical; what I do is behavioral. Ending the AIDS epidemic is going to require integrating the behavioral and the biomedical.
Biomedical interventions alone will not get the job done. We need an educated AIDS workforce to help people like me understand why the treatment is important and to help us stay on treatment when the going gets rough. Doctors can't do that. Only people in the communities most affected can deliver that kind of service.
The late Dr. Maya Angelou said, "When we know better, we do better." This report looks at what the HIV/AIDS workforce needs to knows to do better and makes bold recommendations on how to address the problem.
We also run a story about what can happen when a healthcare provider—in this case, a doctor—is knowledgeable about biomedical interventions. NASTAD's Blake Rowley shares his encounter with a physician who helped him decide to go on PrEP to dramatically reduce the likelihood that he will acquire HIV.
Finally, you have only 10 days left to sign up for health insurance at HealthCare.gov.
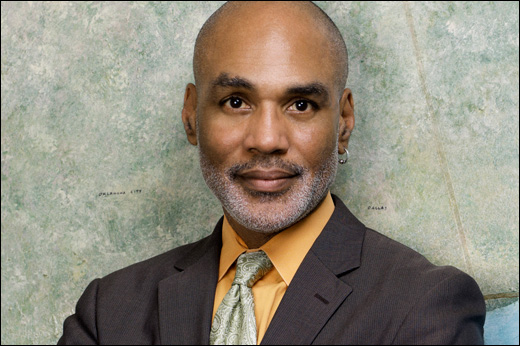
Yours in the struggle,
Phill